-
The Primary Role of a Gastroenterologist
posted: Nov. 07, 2023.

-
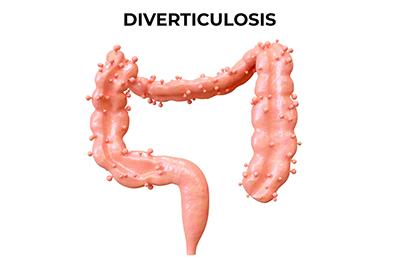
What Is Diverticulosis?
posted: Apr. 10, 2023.
-
Common Dietary Triggers of Digestive Issues: Identifying and Managing Your Triggers
posted: Mar. 23, 2023.

-
Colon Cancer Prevention: Identifying Warning Signs and Reducing Your Risk
posted: Mar. 14, 2023.

This website includes materials that are protected by copyright, or other proprietary rights. Transmission or reproduction of protected items beyond that allowed by fair use, as defined in the copyright laws, requires the written permission of the copyright owners.
