-
Liver Health: Preventive Measures and Lifestyle Changes to Support Liver Function
posted: Apr. 17, 2024.

-
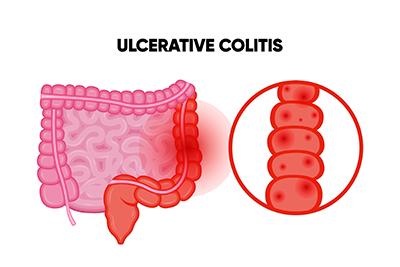
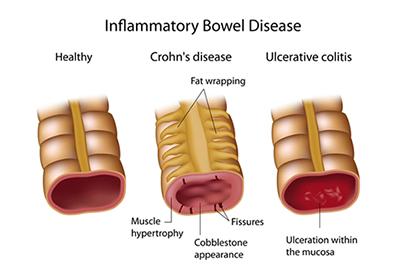
Ulcerative Colitis and Other Digestive Complications
posted: Apr. 01, 2024.
-
Treating Internal Hemorrhoids
posted: Mar. 18, 2024.

-
Three Signs of GERD
posted: Mar. 01, 2024.

-
Are You Dealing With Irritable Bowel Syndrome?
posted: Feb. 15, 2024.

-
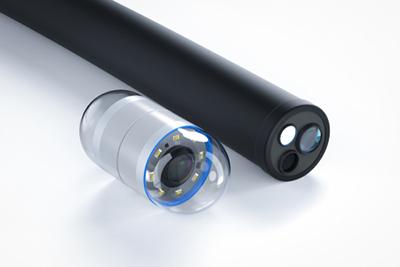
Colon Cancer Screening: Understanding Colonoscopies and Other Methods
posted: Feb. 01, 2024.
-
Inflammatory Bowel Disease (IBD): Understanding Crohn's Disease and Ulcerative Colitis
posted: Jan. 16, 2024.
-
What Causes Acid Reflux?
posted: Jan. 01, 2024.

-
Colon Cancer Screening FAQs
posted: Dec. 07, 2023.

-
Don’t Ignore Your Acid Reflux
posted: Dec. 01, 2023.

-
When Is an Endoscopy Needed?
posted: Nov. 09, 2023.

-
The Primary Role of a Gastroenterologist
posted: Nov. 07, 2023.

-
Choosing Us as Your Gastroenterologist
posted: Oct. 10, 2023.

-
Healthy Eating Habits for a Happy Gut
posted: Oct. 04, 2023.

-
What Are the Symptoms of GERD?
posted: Sep. 15, 2023.

-
Don't Ignore Abdominal Pain
posted: Sep. 01, 2023.

This website includes materials that are protected by copyright, or other proprietary rights. Transmission or reproduction of protected items beyond that allowed by fair use, as defined in the copyright laws, requires the written permission of the copyright owners.
